Services
BPH (Enlarged Prostate)

Benign Prostatic Hyperplasia, or BPH, refers to non-cancerous growth of the prostate.
Benign prostatic hyperplasia (BPH) refers to benign (non-cancerous) growth of the prostate. The prostate begins growing after the age of 25, and this continues throughout men’s lives. BPH essentially refers to growth that causes issues urinating.
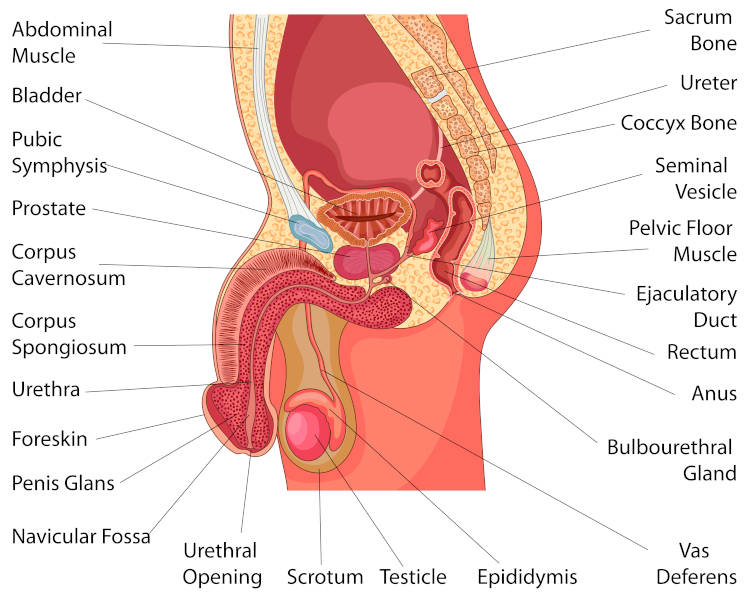
As the gland enlarges, it can squeeze the urethra. The bladder wall becomes thicker, and if this is not addressed, it can lose the ability to empty fully. Urine then remains in the bladder. These problems cause many of the lower urinary tract symptoms (LUTS) of BPH. If you are not able to pass urine at all (urinary retention) or if there is damage to the kidneys, immediate attention is required.
BPH is not related to prostate cancer, nor does it lead to cancer. Still, BPH and cancer can happen at the same time, and screening for prostate cancer is usually done at the same time. BPH itself may not require any treatment, but if it begins to cause symptoms, treatment may help. BPH is very common, and increases with age – about half of all men between ages 51 and 60 have BPH. Up to 90% of men over age 80 have this.

What Does the Prostate Do?
The prostate is part of the male reproductive system and its main job is to make fluid for semen. It is about the size of a walnut and weighs an ounce or so. It sits below the bladder and in front of the rectum. It goes around a tube called the urethra. The urethra carries urine from the bladder and out through the penis.
Symptoms
When the prostate is enlarged, it can block the bladder, or make the bladder work harder in order to empty urine. Frequent urination is a common symptom of BPH. This can be during the daytime, nighttime (nocturia) or both.
Other symptoms include:
- Incomplete emptying: the feeling your bladder is full, even after urinating
- Frequency: the need to urinate frequently
- Intermittency: the need to stop and start several times when passing urine
- Urgency: feeling the urgent need to pass urine, as if you can’t wait
- Weak stream: a weak urine flow
- Straining: trouble starting to pass urine or the need to push or strain to pass urine
- Nocturia: the need to wake up at night more than two times to pass urine
If BPH becomes severe, you might not be able to urinate at all. This may require a urinary catheter to bypass the blockage, and further treatment may be warranted.
How Can BPH Affect Your Life?
In most men, BPH gets worse with age. It can lead to bladder damage and infection if more severe. If left untreated for a prolonged period, the bladder may not squeeze adequately, and a catheter may be required.
Causes
The causes of BPH are not clear. The incidence of BPH increases as men age. Hormone changes are thought to play a role, as are genetics.
Who is at Risk for BPH?
There are many risk factors for BPH. Men who are at a higher risk include:
- Men over the age of 50, as the risk for BPH rises with age
- Men whose fathers had BPH
- Men who are overweight or obese
Can BPH be Prevented?
There is no sure way to prevent BPH. Still, losing weight and eating a well-balanced diet, rich in fruits and vegetables, may help. Too much body fat may increase hormone levels and other factors in the blood and stimulate the growth of prostate cells. Staying active also helps control weight and hormone levels.
Read our Urology of Indiana BPH brochure.
See your doctor if you have symptoms that might be BPH. Also, see your doctor right away if you have blood in your urine, pain or burning when you urinate or if you cannot urinate.
There are many tests for BPH. The following tests are used to diagnose and track BPH.
Symptom Score Index
If you have any urinary changes or symptoms, your doctor may talk to you about the BPH Symptom Score Index. The American Urological Association (AUA) developed this test to assess urinary symptoms.
This is often the first step to diagnose BPH. The score can rate BPH as being mild to severe. You and your health care provider may talk about your results and your medical history. This is sometimes also called the International Prostate Symptom Score (IPSS).
We frequently use this questionnaire at Urology of Indiana to assess where your symptoms are, and whether they are improving or worsening with treatment.
Physical Exam
A digital rectal exam (DRE) is often the next step. During a DRE, you lie on your side or bend over. The doctor inserts a gloved, lubricated finger into your rectum to feel the back wall of the prostate gland. The healthcare provider is looking for enlargement, tenderness, lumps or hard spots. This 10-15 second exam is an important way to find problems. This also assists in screening for prostate cancer.
Urine Tests
These tests are done to measure how well you release urine. This shows the doctor if the urethra is blocked or obstructed. There are several types:
- Urinalysis tests your urine sample to check for important things such as blood, signs of infection, glucose (sugar), protein and other factors that can tell your urologist the cause of your symptoms. Urine tests are also used to screen for bladder cancer. If you have blood in your urine, pain or burning when you pass urine, or you cannot pass urine, it is important to see your doctor right away.
- Post-Void Residual Volume (PVR) measures urine left in the bladder after passing urine. This is a non-invasive test in which an ultrasound probe is placed on the abdomen and a measurement of the amount of urine is taken. This is painless and takes less than a minute.
- Uroflowmetry measures how fast urine flows. This is done when the patient urinates through a sensor to determine the rate of urine flow. This is non-invasive and helps to determine if a blockage is occurring.
- Urodynamics involve the placement of a catheter in the bladder to determine how well the bladder contracts, and whether a blockage exists. These give more information than Uroflow testing, though are slightly more invasive in that they require placement of a catheter.
- Transrectal ultrasound (TRUS) is an ultrasound probe placed in the rectum. This is primarily done to measure the size of the prostate, which can help determine which treatment options are appropriate.
- Cystoscopy is a thin scope that goes into the urethra and into the bladder. Numbing lubricated jelly is placed in the urethra – the test lasts several minutes and helps gain useful information about the prostate anatomy, size and degree of obstruction. We are also able to assess the health of your bladder at this time as well.
- Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) are more detailed scans. Sometimes these are done prior to surgery for BPH. However, if you have had these done for other reasons, they may assist in determining the size and anatomy of the prostate as well.
Treatment
There are many options for treating BPH. You and your doctor will decide together which treatment is right for you. Mild cases may need no treatment at all. In some cases, minimally invasive procedures (surgery without anesthesia) are good choices. And, sometimes a combination of treatments is used.
Medication
Alpha Blockers
Alpha blockers are pills used to relax the muscles of the prostate and bladder neck to reduce BPH symptoms and improve urine flow.
They do not shrink the prostate but they may improve urine flow if there is a blockage. One benefit of alpha blockers is they start to work right away. Side effects may include dizziness, lightheadedness, fatigue and dry ejaculate. Men with moderate to severe BPH and men who are bothered by their symptoms are good candidates. Alpha blockers may not be a good choice if you plan to have cataract surgery soon.
Alpha-blocking drugs include alfuzosin, doxazosin, silodosin, tamsulosin and terazosin.
5-Alpha Reducatase Inhibitors
5-alpha reductase inhibitors are pills that can increase urine flow and shrink the prostate by blocking DHT. This is a male hormone that can build up in the prostate and may cause prostate growth. These drugs may lower the risk of BPH problems and the need for surgery. Side effects include erectile dysfunction and reduced libido (sex drive). You must keep taking the pills to prevent symptoms from coming back. These may be best for men with very large prostate glands.
These prescription drugs may take many months to become fully effective.
Phosphodiesterase Inhibitors
PDE5 inhibitors such as tadalafil (Cialis) have been shown to improve BPH symptoms when taken at a low dose every day. These are also prescribed for erectile dysfunction and may help in this regard as well.
Less Invasive Surgery
Less invasive surgery or minimally invasive surgical treatments (MIST) can often be done as an outpatient, without a stay in the hospital. Recovery time is usually quicker, and recovery is generally faster. It can offer relief from symptoms, including urine control problems, though the risk of needing repeat surgery in the future or continuing medication may be higher than more invasive options. Good candidates tend to be patients with less severe symptoms, or those in whom more invasive options pose an increase risk.
Less Invasive Surgeries
PAE (Prostate Artery Embolization)
Prostate Artery Embolism (PAE) is an interventional radiology procedure in which blood supply is cut off to the prostate (embolized). Decreased blood flow results in shrinking of the prostate, reducing obstruction and relieving urinary symptoms. PAE is performed through a small catheter inserted in the wrist or groin and done under “Twilight or sleep” sedation.
This procedure is done at our Urology of Indiana Interventional Radiology Center, and patients are discharged home the same day. PAE was previously utilized for significant urinary bleeding (hematuria) but has been used more recently for the treatment of prostatic enlargement (BPH). Depending on many clinical factors, this may be a good option to treat patients’ prostate enlargement and urinary symptoms.
Prostatic Urethral Lift (PUL; Urolift)
PUL uses a needle to place tiny implants in the prostate. These implants lift and compress the enlarged prostate so that it no longer blocks the urethra. PUL may be done with either local or general anesthesia.
With this treatment there are no cuts in the body, and tissue is not destroyed or removed. Recovery time is generally less than other forms of treatment, and ejaculatory dysfunction following the procedure is low. Despite this, only certain prostate sizes and anatomy are favorable.
Water Vapor Thermal Therapy (Rezum)
This treatment uses water vapor (steam) to destroy prostate cells squeezing the urethra.
This treatment can be done in a doctor’s office with local anesthesia or after you have taken a pill for pain. It can also be done under sedation if needed. A small cystoscope is placed into the urethra, and a needle is used to inject water vapor into the prostate. This causes prostate cells to shrink and ultimately die, relieving the blockage. The body’s natural healing response then breaks down and removes the dead tissue, causing the prostate to shrink.
Men may be good candidates if they do not want to take medication for BPH or if they have tried prescription drugs and found they do not work. Men who prefer not to have surgery or want to avoid ejaculatory dysfunction may also be good candidates.
Patients usually have a catheter in the bladder for several days following the procedure, and healing time usually lasts several months.
Surgical Options
Photoselective Vaporization of the Prostate (PVP)
Photoselective Vaporization Therapy (also referred to as GreenLight Laser Therapy) is a minimally invasive procedure that uses a special high-energy laser to vaporize excess prostate tissue and seal the treated area. The procedure is performed on an outpatient basis in a surgery center or hospital under spinal block or general anesthesia. PVP typically takes between 30 and 60 minutes to perform, depending on prostate size, and patients are usually discharged within a few hours. Many patients do not require a catheter after PVP, and those who do typically are catheterized for less than 24 hours.
GreenLight Therapy can help provide immediate relief from enlarged prostate symptoms such as frequent urination (especially at night), weak urine flow, urgency and incomplete bladder emptying. It uses laser energy to vaporize the enlarged tissue, creating an open channel for urine to pass through the urethra. Additionally, GreenLight Laser Therapy requires no incisions and typically has no overall negative impact on sexual function.
Urology of Indiana Board Certified Urologist, Scott C. Pike, MD, has been designated as the first Center of Excellence for Photoselective Vaporization of the Prostate (PVP) in the state of Indiana. The Center of Excellence designation recognizes Dr. Pike’s high degree of experience with GreenLight Laser Therapy and a commitment to delivering effective, long-lasting therapy to men suffering from Benign Prostatic Hyperplasia.
Transurethral Resection of the Prostate (TURP)
TURP is a common surgery for BPH. TURP uses an electrocautery loop to shave down the prostate. This is done under anesthesia, and patients may be observed overnight in the hospital. A catheter is usually left in place for several days following the procedure.
Holmium Laser Enucleation of Prostate (HoLEP)
A HoLEP is performed through the urethra, and does not require incision – very similar to the TURP procedure. During a HoLEP, a laser is used to core out prostate tissue to remove obstruction. A common analogy is removing the orange slices and leaving the peel behind. This can be done as an outpatient, but also may require an overnight stay in the hospital. Catheters are left in place for several days following the procedure.
Men with larger prostates who wish to avoid more-invasive surgery may be good candidates for this treatment, though this can be done on any size prostate. This generally removes the most prostate tissue, and is considered a very durable procedure with low re-treatment rates.
Transurethral Water–Jet Ablation (Aquablation)
TWJA uses high-pressure water jets to destroy excess prostate tissue. The surgeon first uses ultrasound to precisely map the location of the excess tissue. Then the high-pressure water jets are directed to that area. Following this, the surgeon inserts another instrument to seal small blood vessels to reduce the risk of bleeding. The patient needs to stay in the hospital one night to irrigate the bladder to prevent blood clots. You may need to use a catheter for about 48 hours after the procedure and should be able to go home the next day.
Single Port Transvesical Prostatectomy
Single Port Transvesical Prostatectomy is a leading-edge surgical procedure using the da Vinci robot to perform a sub-total removal of the enlarged prostate gland. The term “single port” refers to the number of incisions made during surgery. Many other urologic surgeons still approach this procedure utilizing multiple ports or in an open abdominal fashion.
With the single port approach, one 3 cm incision is made above the bladder to insert all of the da Vinci surgical instruments needed to perform the procedure. This enables the surgeon to work in an overall smaller space, thus forgoing risks associated with operating in the abdomen.
Patient benefits include shorter hospital stay, less post-operative pain, less blood loss and shorter catheter time compared to multiport or open simple prostatectomy. The durability of the procedure is longer lasting than prostatic artery embolization. It is performed in a hospital and an overnight stay may be required. Some patients, however, may go home the same day as their procedure.